Sports Medicine: Conservatively manage concussions
Think back to when you were a competitive athlete. How many times did you suffer a concussion? None? Once? Twice? More than two times?
How many times did you experience headaches, dizziness or nausea after receiving a blow to the head? Did you have trouble remembering things, or were you confused, or in a fog? If you experienced these symptoms, you probably suffered a concussion, even if you were not formally diagnosed with one.
How many times did your coach ask you, or have you ever asked one of your athletes, “Did you get your bell rung?” Have you ever said that “so-and-so got their head dinged?” Both of these phrases imply that a concussion has occurred, but they do not explain the signs and symptoms that an individual exhibits.1Defining concussion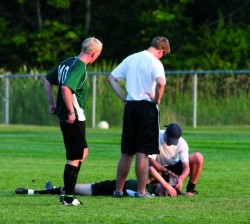
By definition, a concussion is a complex process affecting the brain, induced by traumatic forces.2 Simply put, a concussion is an injury to the brain. The effects of a concussion are subjective in nature, which presents a problem. There isn’t any swelling, discoloration or deformity. Instead, you have to rely completely on what the athlete says is bothering him or her.
Fortunately, the overwhelming majority of concussions (approximately 80 percent) resolve in a short period of time (seven to 10 days). Recovery for a child or adolescent athlete may be longer, due to incomplete brain development.1,2 The strong desire of athletes to participate in their chosen sports often leads to attempts to hide their signs and symptoms related to concussions. This is a dangerous practice, because it can produce susceptibility to a lethal event. Second-impact syndrome occurs when an athlete has sustained a blow to the head that is followed by another blow received prior to resolution of the initial head trauma, which can lead to death. For this reason, conservative management of a concussion is warranted.2
Managing concussions
What can a coach do to ensure proper management of an athlete with a concussion?
First and foremost, insist upon having a properly credentialed athletic trainer (AT) at your school. You would not drive a car without brakes, why would you allow your team to participate without the availability of an athletic trainer? Having an athletic trainer relieves the coach from the primary responsibility for decisions about management of such injuries.
Second, one must recognize the signs and symptoms of a concussion (below). When an athlete relates symptoms of a concussion, take them seriously. Failure to do so may have fatal consequences.2
Along with recognizing the signs and symptoms, be aware that they may not occur immediately; they may develop over several minutes, hours or even days. The referral criteria used to determine if an athlete should consult with a physician or immediate transport to an emergency room is below.1
Third, before allowing an athlete to return to full participation, he or she should be symptom-free for at least seven days.1 Be sure you have obtained written authorization from a physician that clears the athlete for full participation.
Once an athlete is symptom-free, and has been released by a physician, he or she should be gradually progressed to full participation.1,2 At least 24 hours should pass before progression to each subsequent stage of a predetermined protocol
The consequences of the cumulative effects of repetitive concussions are only beginning to be understood. Effects related to cognitive function, academic performance and emotional state are currently the focus of the research.
How repetitive concussions affect individuals at later stages of life is not well-understood. If there is any doubt, have the athlete sit out.
Signs & symptoms of concussions
- Headache
- Pressure in head
- Neck pain
- Nausea or vomiting
- Dizziness
- Blurred vision
- Balance problems
- Sensitivity to light
- Sensitivity to noise
- Feeling slowed down
- Feeling like in a fog
- Dont feel right
- Difficulty concentrating
- Difficulty remembering
- Fatigue or low energy
- Confusion
- Drowsiness
- Trouble falling asleep (if applicable)
- More emotional
- Irritability
- Sadness
- Nervous or anxious
Referral criteria
Day-of-injury referral
- Loss of consciousness on the field
- Amnesia lasting longer than 15 minutes
- Deterioration of neurologic function*
- Decreasing level of consciousness*
- Decrease or irregularity in pulse*
- Increase in blood pressure
- Unequal, dilated or unreactive pupils*
- Cranial nerve deficits
- Any signs or symptoms of associated injuries, spine or skull fracture or bleeding*
- Mental status changes: lethargy, difficulty maintaining arousal, confusion or agitation*
- Seizure activity*
- Vomiting
- Motor deficits subsequent to initial on-field assessment
- Sensory deficits subsequent to initial on-field assessment
- Balance deficits subsequent to initial on-field assessment
- Cranial nerve deficits subsequent to initial on-field assessment
- Post-concussion symptoms that worsen
- Additional post-concussion symptoms as compared with those on the field
- Athlete is still symptomatic at the end of the game (especially at high school level)
Delayed referral (after the day of injury)
- Any of the findings in the day-of-injury referral category
- Post-concussion symptoms worsen or do not improve over time
- Increase in the number of post-concussion symptoms reported
- Post-concussion symptoms begin to interfere with the athletes daily activities (i.e., sleep disturbances or cognitive difficulties)
*Requires that the athlete be transported immediately to the nearest emergency department.
References
1. Guskiewicz KM, Bruce SL, Cantu RC, Ferrara MS, Kelly JP, McCrea M, Putukian M, Valovich McLeod TC. National Athletic Trainers Association Position Statement: Management of Sport-Related Concussion. J Athl Train. 2004;39(3):280297.
2. McCrory P, Meeuwisse W, Johnston K, Dvorak J, Aubry M, Molloy M, Cantu R. Consensus Statement on Concussion in Sport: the 3rd International Conference on Concussion in Sport held in Zurich, November 2008. Br. J. Sports Med. 2009; 43(Suppl I):i76i84.
Gary Wilkerson, EdD, ATC; Marisa Colston, PhD, ATC; and Todd Bullard, MS, ATC, are from the Department of Health & Human Performance at the University of Tennessee at Chattanooga.





